- Home
- Foot & Ankle Conditions
- Sports Injuries
- Achilles Tedonitis and Tendonosis
Achilles Tedonitis and Tendonosis
- Published 10/31/2023
- Last Reviewed 11/1/2023
Dr. Baravarian explains the difference between Achilles Tendonitis, tendinosis, and a rupture
What are Achilles Tendinitis and Achilles Tendinosis?
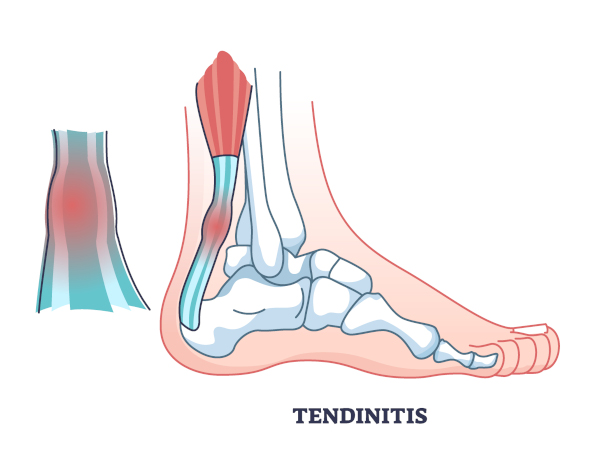
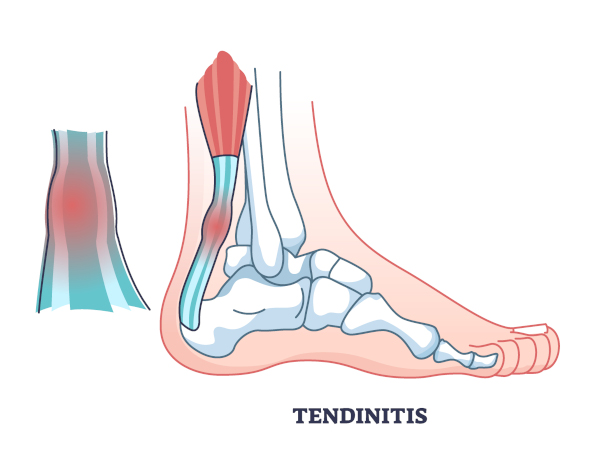
The Achilles tendon (calcaneal tendon) is one of the longest tendons in your body, extending from your calf muscles to the heel bone. Achilles tendinitis is a common overuse injury that results in inflammation of the tendon. This overuse injury results from repetitive stress to the tendon.
Achilles tendinitis vs. tendinosis: what's the difference?
Achilles tendinosis is very similar to tendinitis with one critical difference: it has now become a chronic condition, usually because the injury wasn’t properly treated early on. When the condition progresses to degeneration, thickening of the tendon along with scar tissue can occur, resulting in partial tearing of the tendon fibers. At this point, without medical intervention, the pain will remain or get worse over time.
- What are the symptoms of Achilles tendinitis?
- What causes Achilles tendinitis?
- How do the podiatrists at University Foot & Ankle Institute diagnose an Achilles injury?
- What are conservative treatments for Achilles tendinitis?
- Advanced non-invasive treatments For Achilles tendinosis
- Surgery options for Achilles tendon repair
- UFAI's Achilles Tendinitis & Tendinosis Fast Facts
- Why UFAI is the best choice for Calcaneal Tendon injuries
- Achilles Tendinitis FAQs
- Are steroid injections helpful in the treatment of Achilles tendon disorders?
- Do you commonly use ultrasound and magnetic resonance imaging (MRI) to evaluate Achilles pain?
- Can Haglund’s deformity contribute to Achilles tendonitis?
-
ABFAS® Board Certified in Foot and Ankle Surgery and Co-Director of University Foot and Ankle Institute
Board-Certified Podiatric Foot and Ankle Specialist, Dr. Gary Briskin, DPM, FACFAS, began his medical training by serving a residency at Flint General Hospital in Michigan. Once completed, he established a practice in Century City Hospital, where he soon became chief of podiatric surgery.
Dr. Briskin is a Diplomat of the American Board of Podiatric Surgery and a Fellow of the American College of Foot and Ankle Surgeons. He also serves as an assistant clinical professor at the UCLA School of Medicine and is co-founder and co-director of University Foot and Ankle Institute.
Read Our Achilles Tendon Blog Articles
- An Inside Look at Shockwave Therapy for Heel Pain, now available in Valencia, CA
- Avoiding Foot and Ankle Overuse Injuries While Dog Walking
- How Carrying Extra Weight Affects Your Feet and Ankles
- What's Plantar Tendonitis and Why is it Still a "Medical Mystery"?
- Got Plantar Fasciitis or Achilles Tendonitis? Could PRP, Amniox Stem Cells or Cortisone Answer Your Pain Relief Prayers?
- Your Lower Back Pain May Be Caused By How You Walk
- Common Prescriptions and OTC Medications That Affect Your Feet and Certain Foot and Ankle Conditions
- Achilles Tendinitis Treatment Do’s and Don’ts
- Beat the 6 Most Common Walking Pains
 I’m very happy with the care and concern the staff and Dr. Franson have shown towards me throughout my surgery and aftercare. D...Coleen R.
I’m very happy with the care and concern the staff and Dr. Franson have shown towards me throughout my surgery and aftercare. D...Coleen R. Please provide handicap parkingBarry S.
Please provide handicap parkingBarry S. Dr. Ambibola Johnson is awesome!Laurie S.
Dr. Ambibola Johnson is awesome!Laurie S. I appreciate the care and timeliness of all my appointments I’ve had at UFAI. Gray, Lydia and the staff all are wonderful. Lydi...Edelmira G.
I appreciate the care and timeliness of all my appointments I’ve had at UFAI. Gray, Lydia and the staff all are wonderful. Lydi...Edelmira G. I have been a patient of Dr. Johnson for over a year. He is an excellent podiatrist and podiatric surgeon. The quality of my l...William B.
I have been a patient of Dr. Johnson for over a year. He is an excellent podiatrist and podiatric surgeon. The quality of my l...William B. Very greatfull for the doctor and stuffJesus M.
Very greatfull for the doctor and stuffJesus M. Doctor was very caringBrigitte S.
Doctor was very caringBrigitte S. Everyone is very nice and efficient-
Everyone is very nice and efficient-
Especially Dr Kelman. He takes very good care of me!!Claudia K. Great costumer service.
Great costumer service.
Prompt and efficientDean W. I recommend without reservation the incredible team at University Foot and Ankle and their Physical Therapy department at their...Jeff K.
I recommend without reservation the incredible team at University Foot and Ankle and their Physical Therapy department at their...Jeff K. No . I’m pleased with the care .Michael P.
No . I’m pleased with the care .Michael P. Appreciate the professionalism and expertise, as well as the caring.Stella G.
Appreciate the professionalism and expertise, as well as the caring.Stella G.
-
 Achilles Tendinitis Treatment Do’s and Don’ts
Read More
Achilles Tendinitis Treatment Do’s and Don’ts
Read More
-
 Listen Now
Avoiding Foot and Ankle Overuse Injuries While Dog Walking
Read More
Listen Now
Avoiding Foot and Ankle Overuse Injuries While Dog Walking
Read More
-
 Listen Now
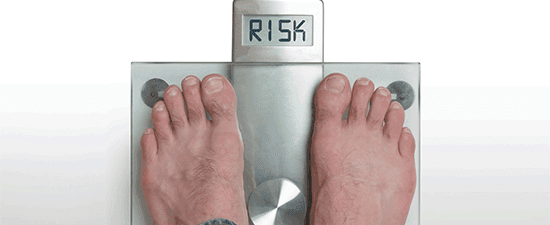
How Carrying Extra Weight Affects Your Feet and Ankles
Read More
Listen Now
How Carrying Extra Weight Affects Your Feet and Ankles
Read More
-
 Got Plantar Fasciitis or Achilles Tendonitis? Could PRP, Amniox Stem Cells or Cortisone Answer Your Pain Relief Prayers?
Read More
Got Plantar Fasciitis or Achilles Tendonitis? Could PRP, Amniox Stem Cells or Cortisone Answer Your Pain Relief Prayers?
Read More
-
 Listen Now
What's Plantar Tendonitis and Why is it Still a "Medical Mystery"?
Read More
Listen Now
What's Plantar Tendonitis and Why is it Still a "Medical Mystery"?
Read More
-
 Listen Now
An Inside Look at Shockwave Therapy for Heel Pain, now available in Valencia, CA
Read More
Listen Now
An Inside Look at Shockwave Therapy for Heel Pain, now available in Valencia, CA
Read More
-
 Listen Now
Common Prescriptions and OTC Medications That Affect Your Feet and Certain Foot and Ankle Conditions
Read More
Listen Now
Common Prescriptions and OTC Medications That Affect Your Feet and Certain Foot and Ankle Conditions
Read More
-
 Listen Now
Beat the 6 Most Common Walking Pains
Read More
Listen Now
Beat the 6 Most Common Walking Pains
Read More
-
 Listen Now
Your Lower Back Pain May Be Caused By How You Walk
Read More
Listen Now
Your Lower Back Pain May Be Caused By How You Walk
Read More